-First episode lasted
for one week 20 years back when she was working in paddy field in month of January which was
relieved on medication .
- for the next 8 years, once a year sob was there for
week again after working in paddy field in January, which was relieved on medication.
-12
years age sob episode lasted for 20 days and she was hospitalized and sob
decreased on treatment -.later for the past 12 years sob episode lasted foe 30
days once a year after working in paddy field in January.
-Last episode was 30 days
back.
The symptomatology suggests that sob is is occurring when she is exposed to paddy.
The anatomical
localization can be at the level of bronchial tubes as evidence of bronchiectasis is
present.
The primary
etiology is exposure to paddy .
Q2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A2) Pharmacological interventions
1)antibiotics are given to treat bronchiectasis
2)inj. Lasik - action:a diuretic is given to decrease the volume overload on lungs there by decreasing pleural effusion
Indications of lasix :pulmonary Edema
Congestive heart failure
Renal diseases
Cirrhosis of liver
Efficacy over placebo :https://journal.chestnet.org/article/S0012-3692(16)35439-3/pdf
3)neb IPRAVENT (ANTICHOLINERGIC BRONCHODILATOR) and BUDECORT(CORTICOSTEROID)
4)tab PULMOCLEAR relieves coughing, congestion and blockade in airways.. efficacy ;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4225926/
nonpharmacological intervention;
-head end elevation: mechanism of action: improves oxygenation, decreases incidence of VAP , increases hemodynamic performance and end expiratory lung volume decreases incidence of aspiration.
Q3)What could be the causes for her current acute exacerbation?
A3)Cause
for current exacerbation can be due the comorbidities as she is a known case of
diabetes since 8 years and diagnosed with hypertension and another cause can be
her age and as it being a chronic problem some part of lung may have been fibrosed.
Q4) Could the ATT have affected her symptoms? If so how?
A4) ATT drugs are known nephrotoxic agents but considering the duration of usage I think ATT has no effect on her symptoms
Q5) What could be the causes for her electrolyte imbalance?
A5)Cause of
her electrolyte imbalance can be kidney dysfunction because of right heart
failure
CNS
CASE2A https://143vibhahegde.blogspot.com/2021/05/wernickes-encephalopathy.html
Q1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A1) - 9 days ago patient started to talk and laugh to himself and there is decreased food intake and also he was unable to move himself off the bed and move around.
-there is also short term memory loss since 9 days
-history of 2-3 episodes of seizures is there 1 year ago recent one being 4 months back.
-the seizure activity which occured 4 months back was after cessation of alcohol intake for 24 hours.
-He is a known case type 2 diabetes mellitus since 2 years and not taking regular medication.
The primary etiology in this patient is related to alcohol withdrawal and the anatomical localization is CNS(brain)
.the symptomatology suggests that patient is having withdrawal symptoms.
Q2)What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A2) pharmacological intervention:
1.Thiamine
mechanism of action:thiamine prevents occurrence of Wernicke encephalopathy which occurs due to deficiency of thiamine I
indications : treatment of beri beri
Neuritis
Ulcerative colitis
to prevent Wernicke encephalopathy
efficacy: Background: Alcohol dependence is associated with severe nutritional and vitamin deficiency. Vitamin B1 (thiamine) deficiency erodes neurological pathways that may influence the ability to drink in moderation. The present study examines tolerability of supplementation using the high-potency thiamine analogue, benfotiamine (BF), and BF’s effects on alcohol consumption in severely affected, self-identified, alcohol dependent subjects. Methods
A randomized, double-blind, placebo-controlled trial was conducted on 120 non-treatment seeking, actively drinking, alcohol dependent men and women volunteers (mean age=47 years) from the Kansas City area who met DSM-IV-TR criteria current alcohol dependence. Subjects were randomized to receive 600 mg benfotiamine or placebo (PL) once daily by mouth for 24 weeks with 6 follow-up assessments scheduled at 4 week intervals. Side effects and daily alcohol consumption were recorded. Results Seventy (58%) subjects completed 24 weeks of study (N=21 women; N=49 men) with overall completion rates of 55% (N=33) for PL and 63% (N=37) for BF groups. No significant adverse events were noted and alcohol consumption decreased significantly for both treatment groups. Alcohol consumption decreased from baseline levels for 9 of 10 BF treated women after 1 month of treatment compared with 2 of 11 on PL. Reductions in total alcohol consumption over 6 months were significantly greater for BF treated women (BF: N=10, −611±380 Std. Dev; PL: N=11, −159±562 Std. Dev, p-value=0.02). ConclusionsBF supplementation of actively drinking alcohol dependent men and women was well-tolerated and may discourage alcohol consumption among women. The results do support expanded studies of BF treatment in alcoholism.
2.lorazepam and pregabalin are given for the neurological symptoms. Benzodiazepines
Benzodiazepines (BZD) are the mainstay of treatment in alcohol withdrawal. Benzodiazepines are safe, effective and the preferred treatment for AWS. Benzodiazepines are cross-tolerant with alcohol and modulate anxiolysis by stimulating GABA-A receptors [24]. During withdrawal from one agent, the other may serve as a substitute. They are proven to reduce withdrawal severity and incidence of both seizures and delirium tremens (DT)
The ideal drug for alcohol withdrawal should have a rapid onset and a long duration of action, a wide margin of safety, a metabolism not dependent on liver function, and absence of abuse potential [43]. Various BZDs offer many of these advantages. BZDs have been found effective in: 1) preventing agitation and alcohol withdrawal seizures; 2) preventing delirium tremens; and 3) as cross-tolerant agents with ethanol. BZDs, owing to their wide margin of safety and low potential to produce physical dependence and tolerance in short-course therapy, are therefore very, effective in the treatment of alcohol-withdrawal syndrome. They are the drugs of choice for alcohol withdrawal
3.PREGABALIN
Mechanism of action:it is analog of neurotransmitter GABA
Indications:-peripheral neuropathic paint like diabetic neuropathy and post hermetic neuropathy
- adjuvant treatment of partial seizures
- management of fibromyalgia
Efficacy of pregabalin
https://pubmed.ncbi.nlm.nih.gov/18553183/
Q3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
A3) The reason can be thiamine, during previous withdrawal the body might have enough thiamine which prevented the occurence of neurological symptoms. During this withdrawal due to thiamine deficiency the neurological symptoms have occured.
Q4) What is the reason for giving thiamine in this patient?
A4)Thiamine is useful in preventing WERNICKE ENCEPHALOPATHY.it is an acute disorder due to thiamine deficiency manifested by confusion, ataxia, ophthalmoplegia, impaired memory and amnesia.
Q5) What is the probable reason for kidney injury in this patient?
A5)Chronic alcoholism can cause acute kidney injury.
Q6)What is the probable cause for the normocytic anemia?
A6)Anemia is common in alcoholics, the person who takes excess alcohol wont eat properly so they will be nutritionally deprived.
Q7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
A7)As mentioned above excess alcohol intake can cause nutritional deficiencies which results in poor wound healing.but per se alcohol does not cause foot ulcer .alcohol is associated with duodenal and gastric ulcers.
CASE 2B
https://kausalyavarma.blogspot.com/2021/05/a-52-year-old-male-with-cerebellar.html?m=1
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A1) symptomatology :patient gave history of giddiness 7 days back with one episode of vomiting which was subsided on taking rest.
again 4 days after he developed giddiness which was associated with 2-3 episodes of vomiting, bilateral hearing loss, aural fullness and tinnitus.
there is also history of postural instability.
2)What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A2)pharmacological interventions:
1.VERTIN ;
Mechanism of action: It is a histamine analog ,it works by increasing blood flow in inner ear.
Indications; Dizziness, vertigo, nausea and vomiting due to motion sickness
Indications: Nausea and vomiting following any surgery/chemotherapy/radiotherapy.
3.ECOSPRIN
Mechanism of action: IT is a NSAID which has anti-platelet effect it prevents clot formation and thus prevents recurrence of stoke.
4.ATORVOSTATIN mechanism of action :it is a statin which controls the levels of cholesterol in the body thus decreasing the atherogenesis and preventing stroke.
Indications: -dyslipidemias
After stroke to prevent recurrence.
5.CLOPIDOGREL
Mechanism of action: it is also an anti-platelet drug, it is inhibitor of platelet activation and aggregation
Indications: IN symptomatic carotid artery stenosis, primary prevention of thromboembolism in atrial fibrillation, during PCI for ACS.
3) Did the patients history of de novo HTN contribute to his current condition?
A3) Yes, HYPERTENSION IS A RISK FACTOR FOR STROKE.
4)Does the patients history of alcoholism make him more susceptible to ischemic or haemorrhagic type of stroke?
A4)Even alcohol is also a risk factor for stroke.
CASE 2C http://bejugamomnivasguptha.blogspot.com/2021/05/a-45-years-old-female-patient-with.html
Questions:
1)What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A1)-patient developed bilateral pedal edema 8 months back which is present in both sitting and standing position
-she has pain since 6 days radiating to left limb which was dragging in nature.
-she also had palpitations since 5 days . chest pain and heaviness is also present.
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
A2)as the patient do not have diarrhea or vomiting may be inadequate dietary intake or excess loss through kidney can cause recurrent hypokalemia. the patient also has pedal edema which can be suggestive of kidney malfunctioning.
3)What are the changes seen in ECG in case of hypokalemia and associated symptoms?
3A)ECG changes in hypokalemia include inversion of T wave, QT interval prolongation, visible U wave and mild ST depression .if there is severe hypokalemia arrhythmias like Torsades de points and ventricular tachycardia.
CASE 2D
https://rishikoundinya.blogspot.com/2021/05/55years-old-patient-with-seizures.html
QUESTIONS:
1) Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
A1)Yes.
2) In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
A2)The previous episodes can be caused only due to increased electrical activity ,in present episode there is associated CVA.
CASE 2E https://nikhilasampathkumar.blogspot.com/2021/05/a-48-year-old-male-with-seizures-and.html?m=1
Questions:
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
1A) Damage from alcohol is a common cause of cerebellar ataxia. In patients with alcohol related ataxia, the symptoms affect gait (walking) and lower limbs more than arms and speech. So alcohol may be reason for his ataxia
https://publicdocuments.sth.nhs.uk/pil3307.pdf
2)What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
A2) Liver damage due to too much alcohol can stop the liver from synthesis of coagulants , this may be the reason for his IC bleed
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1341444/#:~:text=The%20impaired%20platelet%20function%2C%20together,associated%20with%20excessive%20alcohol%20intake.
CASE 2F http://shivanireddymedicalcasediscussion.blogspot.com/2021/05/a-30-yr-old-male-patient-with-weakness.html
Questions
1)Does the patient's history of road traffic accident have any role in his present condition?
A1) stroke is a sudden pathology (past accidents not involving head have no effect in stroke)
2)What are warning signs of CVA?
A2)- sudden numbness or weakness of face ,arms ,leg mainly involving only one side
-sudden severe headache
-sudden loss of balance/loss of coordination
-sudden ophthalmoplegia in one or both eyes
-sudden trouble in speaking
-sudden confusion or not not understanding things.
3)What is the drug rationale in CVA?
4)Does alcohol has any role in his attack?
A4)yes alcohol consumption is a risk factor for stroke.
5)Does his lipid profile has any role for his attack??
A5)His lipid profile is normal except for the fact that HDL levels are low,HDL has protective action against stroke.
CASE 2G https://amishajaiswal03eloggm.blogspot.com/2021/05/a-50-year-old-patient-with-cervical.html
Questions*
1)What is myelopathy hand ?
A1)Loss of power of adduction and extension of the ulnar 2/3 fingers and inability to grasp and release rapidly with these fingers.
2)What is finger escape ?
3)What is Hoffman’s reflex?
A3)Involuntary movements of the thumb and index fingers when the examiner flicks the finger nail of middle finger.The following are the steps to hoffmans reflex.

Q1) What can be the cause of her condition ?
A1)According to MRI , cortical vein thrombosis might be the cause of her seizures
Q2) What are the risk factors for cortical vein thrombosis?
A2)Infections: Meningitis, otitis, mastoiditis
Prothrombotic states: Pregnancy, puerperium, antithrombin deficiency protienic and protein s deficiency, Hormone replacement therapy.
Mechanical: Head trauma, lumbar puncture
Inflammatory :SLE ,sarcoidosis ,Inflammatory bowel disease.
Malignancy.
Dehydration
Nephrotic syndrome
Drugs :Oral contraceptives ,steroids, Inhibitors of angiogenesis
Chemotherapy: Cyclosporine and l asparaginase
Hematological: Myeloproliferative Malignancies, Primary and secondary polycythemia
Intracranial :Dural fistula,
Vasculitis: Behcets disease wegeners granulomatosis
Q3)There was seizure free period in between but again sudden episode of GTCS why? Resolved spontaneously why?
A3)Seizures are resolved and seizure free period got achieved after medical intervention but sudden episode of seizure was may be due to any persistence of excitable foci by abnormal firing of neurons.
Q4)What drug was used in suspicion of cortical venous sinus thrombosis?
A4)Anticoagulants are used for the prevention of harmful blood clots.
Clexane ( enoxaparin) low molecular weight heparin binds and potentiates antithrombin three a serine protease Inhibitor to form complex and irreversibly inactivates factor xa.
Risk factors for cortical vein thrombosis
CVS
CASE3A https://muskaangoyal.blogspot.com/2021/05/a-78year-old-male-with-shortness-of.html
Q1)What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
A1)Preserved ejection also known as diastolic heart failure where as reduced ejection fraction heart failure is known as systolic heart failure.
Q2)Why haven't we done pericardiocentesis in this patient?
A2)Here the patient only has acute pericarditis where the effusion is less than that of a tamponade ,the 2D echo suggests absence of tamponade so pericardiocentesis is not done.
Q3)What are the risk factors for development of heart failure in the patient?
A3)Pericardium looses its elasticity in pericarditis and becomes rigid over time, so it does not transfer the intrathoracic pressure changes to the heart there by resulting heart failure.
Q4)What could be the cause for hypotension in this patient?
A4)Heart failure can be cause of hypotension in this patient.
CASE3B https://muskaangoyal.blogspot.com/2021/05/a-73-year-old-male-patient-with-pedal.html
Questions:
1)What are the possible causes for heart failure in this patient?
A1)Chronic hypertension can be the cause of heart failure in this patient.
2)what is the reason for anemia in this case?
A2)Anemia is considered to be frequent comorbidity of heart failure.
3)What is the reason for blebs and non healing ulcer in the legs of this patient?
A3)The cause for nonhealing ulcer is diabetes (hyperglycemia impairs the healing process)
4)What sequence of stages of diabetes has been noted in this patient?
A4)Diabetes leading to macrovascular complication in the form of foot ulcer.
CASE 3C https://preityarlagadda.blogspot.com/2021/05/biatrial-thrombus-in-52yr-old-male.html
Q1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A1)- the patient presented with short ness of breath which progressed from grade 2 to grade 4
-patient also complained of oliguria since two days and anuria since morning.
Q2)What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A2)1.DOBUTAMINE
mechanism of action: It is an inotropic drug
Indications: cardiogenic shock, severe congestive cardiac failure, hypo perfusion if associated with increased peripheral vascular resistance.
2.UNFRACTIONED HEPARIN
:mechanism of action: it inactivates thrombin and factor X through an antithrombin dependent mechanism.
Indications: atrial fibrillation with embolization ,treatment of acute and chronic consumptive coagulopathies like DIC , prophylaxis and treatment of venous thromboembolism, prevention of clotting in arterial and cardiac surgery.
3.CARVEDILOL
Mechanism of action; it is a non selective adrenergic blocker
Indication: heart failure with reduced ejection fraction, hypertension, left ventricular dysfunction following MI.
4.ACETYLE CYSTEIN
Mechanism of action:It increases the synthesis of glutathione in liver , glutathione acts as an antioxidant
Indication:it is used in paracetamol overdosing, to relive chest congestion due to thickened mucous in cystic fibrosis, asthma, bronchitis.
Q3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
TYPE 4 CRS is seen in this patient.
Q4) What are the risk factors for atherosclerosis in this patient?
A4)Hypertension accelerates the process of atherogenesis.
Q5)Why was the patient asked to get those APTT, INR tests for review?
A5)INR is used to determine the effect of oral anticoagulants
aptt test is done to know how well the clotting factors are working.
CASE 3D https://daddalavineeshachowdary.blogspot.com/2021/05/67-year-old-patient-with-acute-coronary.html?m=1
Q1)What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A1) EVOLUTION OF SYMTOMATOLOGY
Diabetes since 12 years
heart burn like episodes since 1 year but it relieved
pulmonary TB 7 months back --treatment took now she is sputum negative
hypertension since 6 months --on medications
SOB since half an hour on day of admission to hospital
ANATOMICAL LOCATION OF PROBLEM: Cardio vascular system
PRIMARY ETIOLOGY OF PATIENT PROBLEM: atherosclerosis --plague formation [hypertension+ diabetes]
Q2)What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A2)Pharmacological interventions:
TAB MET XL 25 MG/STAT-contains Metoprolol as active ingredient
:mechanism of action ;
METOPROLOL is a cardio selective beta blocker
Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline. Beta blockers cause your heart to beat more slowly( negative chronotropic effect)
and with less force( negative inotropic effect). Beta blockers also help open up your veins and arteries to improve blood flow.
Indications:
it is used to treat Angina, High blood pressure and to lower the risk of hear attacks .
Efficacy studies:
Patients were randomized to one of four treatment arms: placebo or ER metoprolol (0.2 mg/kg, 1.0 mg/kg, or 2.0 mg/kg). Data were analyzed on 140 intent-to-treat patients.
Outcome :
mean baseline BP was 132/78 +/- 9/9 mmHg. Following 4 weeks of treatment, mean changes in sitting BP were: placebo = -1.9/-2.1 mmHg; ER metoprolol 0.2 mg/kg = -5.2/-3.1 mmHg; 1.0 mg/kg = -7.7/-4.9 mmHg; 2.0 mg/kg = -6.3/-7.5 mmHg. Compared with placebo, ER metoprolol significantly reduced systolic blood pressure (SBP) at the 1.0 and 2.0 mg/kg dose (P = .027 and P = .049, respectively), reduced diastolic blood pressure (DBP) at the 2.0 mg/kg dose (P = .017), and showed a statistically significant dose response relationship for the placebo-corrected change in DBP from baseline. There were no serious adverse events or adverse events requiring study drug discontinuation among patients receiving active therapy.
Non pharmacological intervention :
PERCUTANEOUS CORONARY INTERVENTION.
Percutaneous Coronary Intervention is a non-surgical procedure that uses a catheter (a thin flexible tube) to place a small structure called a stent to open up blood vessels in the heart that have been narrowed by plaque buildup ( atherosclerosis).
Q3) What are the indications and contraindications for PCI?
INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
High risk stress test findings.
CONTRAINDICATIONS:
Intolerance for oral anti platelets long-term.
Absence of cardiac surgery backup.
Hypercoagulable state.
High-grade chronic kidney disease.
Chronic total occlusion of SVG.
An artery with a diameter of <1.5 mm.
Q4)What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on over testing and overtreatment important to current healthcare systems?
A4) Although PCI is generally a safe procedure , it might cause serious certain complications like
A)Bleeding
B) Blood vessel damage
C) Allergic reaction to the contrast dye used
D) Arrhythmias
E) Need for emergency coronary artery bypass grafting .
Because of all these complications it is better to avoid PCI in patients who do not require it.
OVER TESTING AND OVER TRAETMENT HAVE BECOME COMMMIN IN TODAY’S MEDICAL PRACTICE.
-Research on over testing and overtreatment is important as they are more harmful than useful.
Following are harms to patients:
.Performing screening tests in patients with who at low risk for the disease which is being screened.
For example :Breast Cancer Screenings Can Cause More Harm Than Good in Women Who Are at Low Risk. A harmless lump or bump could incorrectly come up as cancer during routine breast screenings. This means that some women undergo surgery, chemotherapy or radiation for cancer that was never there in the first place.
.Overuse of imaging techniques such as X- RAYS AND CT SCANS as a part of routine investigations.
Overuse of imaging can lead to a diagnosis of a condition that would have otherwise remained irrelevant -
OVERDIAGNOSIS.
Also the adverse effects due to this are more when compared to the benefits.
.Over diagnosis through over testing can psychologically harm the patient.
Hospitalizations for those with chronic conditions who could be treated as outpatients[ can lead to economic burden and a feeling of isolation.
Harms to health care systems:
The use of expensive technologies and machineries are causing burden on health care systems.
CASE 3E
https://bhavaniv.blogspot.com/2021/05/case-discussion-on-myocardial-infarction.html?m=1
Q1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A1)EVOLUTION OF SYMTOMATOLOGY
diabetic since 8 years
hypertension since 8 years
took first dose of COVISHIELD vaccine 5 days back before admn to hospital
chest pain in right side of chest
giddiness and profuse sweating on day of the admission
ANATOMICAL LOCATION OF PROBLEM: cardio vascular system
PRIMARY ETIOLOGY OF PATIENT PROBLEM: as she is diabetic since 8 years that might cause atherosclerosis due to accumulation of fatty and fibrinous material in the walls
Q2)What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A2)Pharmacological interventions:
1.tab ASPIRIN 325 mg
:mechanism of action: inhibits platelet aggregation by interfering with thromboxane in platelets caused by COX 1 inhibition
indications :
to reduce the cardio vascular deaths in suspected case of MI
efficacy:
low dose aspirin each day for atleast10 years lower the risk of cvd by 10% and odds ratio from 0.85 to 0.90
2.tab ATORVASTATIN 80 mg
Mechanism of action :competitive inhibitor of enzyme HMG CO A reductase
indication:
to prevent CV events in patients who are at risk used as preventive agent
efficacy:
studies shown that it decrease LDL cholesterol concentration by61% and triglycerides by 46%
—tab Clopidogrel 300 mg
MOA : Inhibitor of platelet aggregation by binding one of the ADP receptors on platelets
indications:
ACS
recent MI ,recent stroke ,peripheral arterial disease
Q3)Did the secondary PTCA do any good to the patient or was it unnecessary?
A3) Yes it is good to patient, stent was placed and the patient is doing good
CASE 3F https://kattekolasathwik.blogspot.com/2021/05/a-case-of-cardiogenic-shock.h
Q1)How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
A1)May be the rural medical practitioner gave a diuretic which decreased the fluid overload on lungs there by relieving sob.
Q2) What is the rationale of using torsemide in this patient?
A2)Torsemide is used to reduce extra fluid in the body as the heart is already in shock state , any extra fluid in the body worsens the condition of heart.
Q3)Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
GASTROINTESTINAL
Case 4A;
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-pancreatitis-with.html)
Q1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A1)The
symptomatology of patient
-20 days ago severe pain in the right hypochondriac and epigastrium which was sudden in onset, gradually progressive ,and dragging type and radiating to right shoulder.
-fever and loss of appetite since 18days
Fever can
be attributed to acute infective peripancreatic fluid collection.
Anatomical Localization
is pancreas as the symptoms are associated with intake of alcohol PANCREATITIS??
The primary
etiology is alcohol intake
Q2)What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A2) 1.ZOSTUM Inj
Mechanism of action:antibacterial
Indications: used to treat severe and serious bacterial infections such as respiratory tract infection, urinary tract infection, skin and soft tissue infection, joint and bone infection
Efficacy https://www.researchgate.net/publication/303996525_A_Study_on_prescribing_and_cost_pattern_of_antimicrobial_agents_in_a_tertiary_care_teaching_hospital
2.inj METROGYL
Mechanism of action:anti bacterial and anti parasitic
Indications used to treat diarrhoea or dysentery due to parasitic infections such as amoebiasis. It is used to prevent sexually transmitted infections such as urogenital trichomoniasis or giardiasis. It is also used to treat infections of the gums, teeth and skin due to various infective microorganisms
3.ULTRACET
Mechanism of action: centrally acting analgesic
Indications moderate to severe pain
Approach
to treat the patient
Antibiotics
given to combact infection
TNP preferred
because of the gastrointestinal symptoms of the patient.
Pleural effusion
should be drained
CASE4B:
https://nehae-logs.blogspot.com/2021/05/case-discussion-on-25-year-old-male.html
Q1)w hat is causing the patient's dyspnea? How is it related to pancreatitis?
A1)Pancreatitis
can cause chemical changes in the body that can effect lung function causing
respiratory symptoms. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4087768/
Q2)Name possible reasons why the patient has developed a state of hyperglycemia.
A2)Chronic
inflammation of the pancreas can damage the beta cells producing insulin which
can lead development of diabetic state
And also
diabetes and pancreatitis have some risk factors in common like alcohol
Q3)What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
A3)Fatty
liver changes are seen in patients with pancreatitis and the patient being a alcoholic
some fatty changes can already be present.
An ALT to
AST ratio over 2 is highly suggestive of alcohol liver disease.
Q4)What is the line of treatment in this patient?
A4)Line of
treatment;
i)manage
hyperglycemia and monitor GRBS
ii)ask the
patient to stop alcohol consumption.
CASE 4C; https://chennabhavana.blogspot.com/2021/05/general-medicine-case-discussion-1.html
Q1) what is the most probable diagnosis in this patient?
A1)Probable
diagnosis is hollow viscus perforation and its effects like free fluid and
hematoma formation.
Q2)What was the cause of her death?
A2)Cause of
her death can be as a complication of surgery in the form of pneumonia(As symptom
just before the death are cough and sob) as many people who undergo surgery
already have weakened immune system and they are prone to get infections.
Q3)Does her NSAID abuse have something to do with her condition? How?
A3)Effect
of nsaids abuse ; nsaids are known risk factor for peptic ulcer formation and a
complication of ulcer in git is perforation.so nsaids abuse can have contributed to her disease outcome.
CASE5A https://kavyasamudrala.blogspot.com/2021/05/medicine-case-discussion-this-is-online.html
Q1)What could be the reason for his SOB ?
A1)Reason for his sob can be POST TURP SYNDROME: it occurs because of irrigation of absorption of large volumes of irrigation fluid during turp which can cause HYPONATREMIA,CARDIORESPIRATORY depression.
Q2)Why does he have intermittent episodes of drowsiness ?
A2)The hyponatremia which occurs as a part of post turp syndrome :low levels of sodium in the body can cause lethargy, fatigue and sleep.
Q3)Why did he complaint of fleshy mass like passage in his urine?
A3)Passing of fleshy like mass which is foamy can be because of infection where pus cells are more.
Q4)What are the complications of TURP that he may have had?
A4)Complications of turp can be bladder injury, bleeding, hematuria, dysuria, infection. in this patient it can be infection as pus cells are seen .
CASE 5B https://drsaranyaroshni.blogspot.com/2021/05/an-eight-year-old-with-frequent.html
Q1) Why is the child excessively hyperactive without much of social etiquettes ?
A1)The symptoms of the child point the diagnosis towards ADHD (attention deficit hyperactivity disorder)
Q2)Why doesn't the child have the excessive urge of urination at night time ?
A2)As the child do not have bedwetting nor waking up at night to pass urine it can be a case of receptor over activity effected by gravity(neurogenic overactivity bladder) or pollakiuria(idiopathic frequent urination)it can also be psychosomatic as his mother completely restricted him from using smartphone since 4 months before which he is addicted to ,so the child sleeps normally at night.
Q3)How would you want to manage the patient to relieve him of his symptoms?
A3)First look if any pathology is present in the genitourinary system, then try with the help of psychiatrist find whether it is adhd or not, if yes do cognitive behaviour therapy.
CASE 6A:
Q1)Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
A1)Clinical history and physical findings---
Cough since 2 months on taking food and liquids
difficulty in swallowing since 2 month
H/O weight loss of 10 Kgs since 2 months, hoarseness of voice
Incapable of food intake
Oro pharyngeal regurgitation
Q2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
A2)A retrospective analysis examining all forms of IRIS, 33/132 (25%) of patients exhibited one or more disease episodes after initiation of ART. Other cohort analyses examining all manifestations of IRIS estimate that 17–23% of patients initiating ART will develop the syndrome.
[ INTERVENTION :
The most effective prevention of IRIS would involve initiation of ART before the development of advanced immunosuppression. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/ul.
CASE 7A:
Link to patient details:
Q1)Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors
present in it ? What could be the cause in this patient ?
A1)Yes, it could be due to intake of contaminated toddy
Q2)What is the aetio pathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
A2)According to some studies, alcoholism mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver.
Q3)Is liver abscess more common in right lobe ?
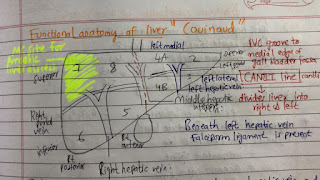
A3)Yes right lobe is involved since the portal circulation drive is more towards the right lobe .
the amoebic liver abscess is more common in the 7th segment (the right postero superior segment) of liver.
Q4)What are the indications for ultrasound guided aspiration of liver abscess ?
A4)Indications for USG guided aspiration of liver abscess
- amoebic liver abscess
-Large abscess more than 6cms
- Left lobe abscess
-Caudate lobe abscess
-Abscess which is not responding to drugs
-seronegative abscess
CASE 7B:Link to patient details:
QUESTIONS:
1)Cause of liver abscess in this patient ?
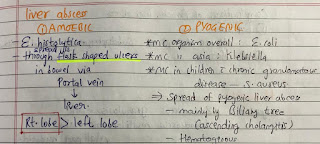
A2)Cause may be due to Entamoeba histolytica. the pyogenic abscesses are usually polymicrobial , most commonly seen organisms are E. coli, Klebsiella, streptococcus, staphylococcus, anaerobes.
1)How do you approach this patient ?
A2)I will approach in the same as given in blog but if abscess rupture emergency laparotomy is to be done.
3)Why do we treat here ; both amoebic and pyogenic liver abscess?
A3)Though the probable diagnosis is amoebic liver abscess its better to give antibiotics to be safe side.
4) Is there a way to confirm the definitive diagnosis in this patient?
A4) USG can be done to see the site of the abscess . USG guided aspiration can be done to confirm diagnosis , but there is risk of perforation .
CASE 8;
Link to patient details:
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A1)3 years ago- diagnosed with hypertension
21 days ago- received vaccination at local PHC which was followed by fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication
18 days ago- complained of similar events and went to the the local hospital, it was not subsided upon taking medication(antipyretics)
11 days ago - c/o Generalized weakness and facial puffiness and periorbital edema. Patient was in a drowsy state
4 days ago- a] patient presented to casualty in altered state with facial puffiness and periorbital edema and weakness of right upper limb and lower limb b.] towards the evening patient periorbital edema progressed c.] serous discharge from the left eye that was blood tinge d.] was diagnosed with diabetes mellitus
patient was referred to a government general hospital
patient died 2 days ago
patient was diagnosed with diabetic ketoacidosis and was unaware that he was diabetic until then. This resulted in poorly controlled blood sugar levels. The patient was diagnosed with acute oro rhino orbital mucormycosis .Rhino cerebral mucormycosis is the most common form of this fungus that occurs in people with uncontrolled diabetes the fungus enters the sinuses from the environment and then the brain.
The patient was also diagnosed with acute infarct in the left frontal and temporal lobe. Mucor mycosis is associated with the occurrence of CVA
https://www.cdc.gov/fungal/diseases/mucormycosis/definition.html
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A2)The proposed management of the patient was –
1. inj. Liposomal amphotericin B according to creatinine clearance
2. 200mg itraconazole was given as it was the only available drug which was adjusted to his creatinine clearance
3.Deoxycholate was the required drug which was unavailable
Reference :https://pubmed.ncbi.nlm.nih.gov/23729001/
I. Management of diabetic ketoacidosis –
(a) Fluid replacement- The fluids will replace those lost through excessive urination, as well as help dilute the excess sugar in blood.
Electrolyte replacement-The absence of insulin can lower the level of several electrolytes in blood. Patient will receive electrolytes through a vein to help keep the heart, muscles and nerve cells functioning normally
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
A3)Mucormycosis, colloquially known as black fungus, is a serious fungal infection that was seen in far smaller numbers in India before Covid-19, too. But it is now affecting post-Covid patients in large numbers. As of May 22, the government has reported 8,848 cases of this fungal infection.
Possible causes could be:
Usage of industrial oxygen???
-use of steroids in the management of COVID-19??
-use of unhygienic masks which are not washed
properly??
CASE 9:Infectious Disease (Covid 19)
As these patients are currently taking up more than 50% of our time we decided to make a separate log link here:
for this question that contains details of many of our covid 19 patients documented over this month and we would like you to:
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe and
3) indicate for each patient, the day of covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe covid (for example, altered sensorium, hypotension etc). Normal sequence in covid
(10) 6th may: previous elogs of our senior batch were shared with us. they gave us an idea of how to do elogs
8th may : covid patient updates were shared along with the CT scan and x ray finding and other investigations which were done. the treatment plan was also discussed .
10th may : a case of liver abscess was discussed
21/M student occasional toddy drinker Came with
H/o pain in the epigastrium & right hypochondrium , loss of appetite & fever from 20 days - diagnosed as liver abscess & got treated outside.
In spite of he was having intermittent pain & fever for which he came to our hospital.
O/E:
Pt C/C/C,PR: 82 bpm, BP: 110/70 mmhg
CVS: S1 S2 + , no murmurs,RS: BAE+ , NVBS
P/A: Soft , NT ,CNS: NFND
Dx:
Liver abscess (segment VII of right lobe with 50 to 60% liquefaction)
And our doubts regarding treatment protocols of Covid were clarified, this discussion helped to clear a lot of doubts regarding Covid treatment.
May 11: the following case was discussed in a great detail
67yrs female
Diagnosis-Viral pnemonia secondary to COVID-19, HTN, HYPOTHYROIDISM, CENTRAL OBESITY, CVA
She was having hypersomnolence in the day time during yesterday's morning rounds.
Later her son told me she had phoned them at 3:00 AM yesterday complaining that there was a man here who was threatening to take her away by morning. We checked the CCTV footage during that time yesterday and didn't find anyone near her bed except she did appear to wake up sometime around that time and was on the phone.
With this case I have understood the neuropsychiatric aspects of COVID .
May 12:updates of Covid cases were given
May 13: an interesting case of 8 year old boy with frequent micturition was discussed
May 14 : differential diagnosis for a 78 year old Male with pericardial effusion was discussed
May 15; a case of ICU psychosis with Covid infection has been discussed
May 16: Covid cases updates where given.
May 17: 2 cardiology cases where discussed along with their elogs. Discussion about percutaneous intervention was done.
May 18: case of tracheo oesophageal fistula with the endoscopic video was shared
In the 2-4 session a session with the attenders of Covid patients with their case discussion was done
May 19: Acute cerebral vascular accident case was shared along with the MRI image findings
May 20: elogs of Covid patients were shared by many students
Going through these elogs which were made by many students helped me to get know about all cases in the hospital ,through elogs we can cover lot of cases.
May 21: a case with differential of Wernicke and withdrawal was discussed and the key points on how to diagnose were put on ex: thiamine administration improves the patient condition in Wernicke’s encephalopathy where as the condition remains same in withdrawal.
May 22: questions regarding the cases in elogs were put up finding answers to these questions helped me to go through many research papers And trials which was very
May 23: some other elogs with questions were shared.
Afternoon session for case discussion was done.
May 24: discussion about stroke score was done
I’ve leaned a new term today
PPCRA - Peripapillary chorioretinal atrophy
This can be seen in myopics and in some cases of glaucoma.
May 25: discussion about granulation tissue formation and its association with healing of an ulcer was done.
May 26: a case of pancreatitis with pleural effusion and case of pemphigus Bulgaria with clinical pictures was posted.
May 27: clinical picture of Ascites in a female was shared
A detailed discussion about usage of antivirals in Covid was done. Efficacy of antivirals with study trials were shared.
May 28: a case of steroid induced Cushing syndrome was shared.


















Comments
Post a Comment