19year old boy with sickle cell crisis and thalasemia
Mallannagari.Srilekha
Roll No:- 77 MBBS 9th-Sem
This is online E log book to discuss out patients de-identified health data shared after taking his guardian`s informed consent. Here we discuss our individual patient`s problems through series of inputs from available global online community of experts with an aim to solve patients clinical problems with collective current best evidence based inputs. This E log book also reflects my patient centered online learning portfolio and your valuable inputs on comments box is welcome.
A 19 year old boy came to the causality with chief complaints of body pains since two days
The patient is a known case of sickle cell anemia and thalasemia (diagnoses 10years back).
Body pains since two days. Pain in the joints mainly in the knees,elbow.ankle.pain in the legs and backache.
There is history of one episode of vomiting 1 day back in the evening after having milk
In 2008 patient has history of jaundice and came here treated for iron deficiency anemia , jarmo globing was 7gm/dl then.later the patient had few episodes of jaundice later as well ,in 2012 patient was advised to HPLC and diagnosed to have sickle test and thalasemia as sickling test is positive and there is high HbA2-4.7% and HbS of 61.3%..
After diagnosis the patient was advised to maintain haemoglobin >10gm/dl, adequate hydration, avoid NSAIDS.
In 2018 the patient had history of bilateral leg pains and chest pain
In 2019 again he had bilateral leg pains
In 2022 he has similar crisis on 17/2/22-cured in 4 days
28/2/22- cured in 6 days
6/3/22- cured in 6 Days
This is the 4th episode this year.
No history of fever,cough,burning micturition
PAST HISTORY:
FAMILY HISTORY:
Father- thalasemia trait
Mother-sickle cell trait
Sister-sickle cell trait
PERSONAL HISTORY
Diet - mixed
Appetite- decreased
Sleep- disturbed due to body pains
Bowel and bladder-regular
No known drug allergies
GENERAL EXAMINATION:
patient is conscious ,coherent, cooperative and oriented to Time, place , person.
Well built and well nourished
Pallor -present
Icterus no
Cyanosis no
Clubbing no
Lymphadenopathy no
Edema no
Vitals
Pulse rate 84 regular , normal volume.
Blood pressure 130/80 mmHg measured in right arm
Respiratory rate18 cpm
Temperature afebrile
Saturation 99% at room air
Systemic examination:
CVS:S1 and S2 heart sounds heard.
No murmurs heard
RESPIRATORY SYSTEM
Position of the trachea central
BAE present , vesicular breath sounds heard
ABDOMINAL EXAMINATION
Slightly distended abdomen
Hernial orifices are free.
No free fluid no bruits
bowel sounds heard
No tenderness
Spleen is palpable and liver is not palpable
CNS examination normal
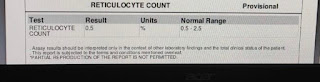
INVESTIGATIONS:
USG abdomen showed slight splenomegaly.
ECG
MANAGEMENT:



Comments
Post a Comment