62 year old Male with shortness of breath and generalised weakness
I have been given this case to solve in an attempt to understand the topic of patient clinical data analysis to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan
Name:M.Srilekha(intern)
Chief complaints:
Generalised weakness since 7 years
Shoulder pain since 2016
Shortness of breath since 5-6 months
lower back pain since 2 months
History of presenting illness:
Patient was apparently normal in 2011 then he had an heart attack for which PTCA was done
Later he developed generalised weakness from 7 years
then he developed shortness of breath Since 5-6 months insidious in onset ,gradually progressing to NHYA grade 2 currently.Aggravated on climbing stairs ,lifting heavy weights . No h/o cough, palpitations, no h/o chest pain, no h/o fever. No h/o decreased urine urine output No h/o pedal edema
On and off back pain which is of pricking type radiating to b/l shoulder and lower back since 6 months relieved on medication.
No h/o decreased range of movements
No h/o trauma
No localised swelling seen
Past history:
PTCA done in 2011
Not a k/c/o hypertension diabetes epilepsy tuberculosis thyroid disorders
H/o malignant malaria 20 years back
Personal history:
Appetite: decreased
Sleep adequate
Bowel and bladder regular
Habits :
Alcohol: used to drink regularly from 2007-2010 then he had heart attack in 2010 so stopped taking alcohol from 2010-2020,now takes occasionally 60ml/day
Tobacco:stopped 10 years back used to smoke 2-4 beedis/day
Family history:
Oral cancer for grand mother
General examination:
patient is conscious coherent and cooperative well oriented to time place and person
No pallor icterus cyanosis clubbing lymphadenopathy edema
Central obesityVitals:
PR:60bpm
BP:120/90
RR:16com
SpO2:98%
GRBS:
CVS:
S1,S2 +
No added murmurs
JVP not elevated
RS:
Inspection:
b/l symmetrical chest both sides moving equally with respiration
Trachea central in position
Auscultation:
BAE + normal vesicular breath sounds heard
Per abdomen:
Soft non tender
No organomegaly
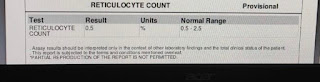
Investigations:
2D echo
Eccentric TR,mild MR AR TR with PAH
Mild global hypokinesia no MS AS sclerotic AV
Fair to good LV function
Diastolic dysfunction + NO PE
ECG:
LFT:
PLSB:
Provisional diagnosis:
SOB under evaluation
Medicines:
Since 6 months Since 6 monthsSince 12 years for acidity
Tobacco:stopped 10 years back used to smoke 2-4 beedis/day
Family history: oral cancer for grand mother
General examination: patient is conscious coherent and cooperative well oriented to time place and person
No pallor icterus cyanosis clubbing lymphadenopathy edema
Vitals:
PR:60bpm
BP:120/90
RR:16com
SpO2:98%
CVS:S1,S2 +,No added murmurs,JVP not elevated
Respiratory system:
Inspection: b/l symmetrical chest both sides moving equally with respiration ,Trachea central in position
Auscultation:BAE + normal vesicular breath sounds heard
Per abdomen:Soft non tender ,No organomegaly
2D echo:Eccentric TR,mild MR AR TR with PAH
Mild global hypokinesia no MS AS sclerotic AV
Fair to good LV function,Diastolic dysfunction + NO PE
6 min walk test:
Vitals before 6 min walk test :
HbA1c:6.4%


















Comments
Post a Comment